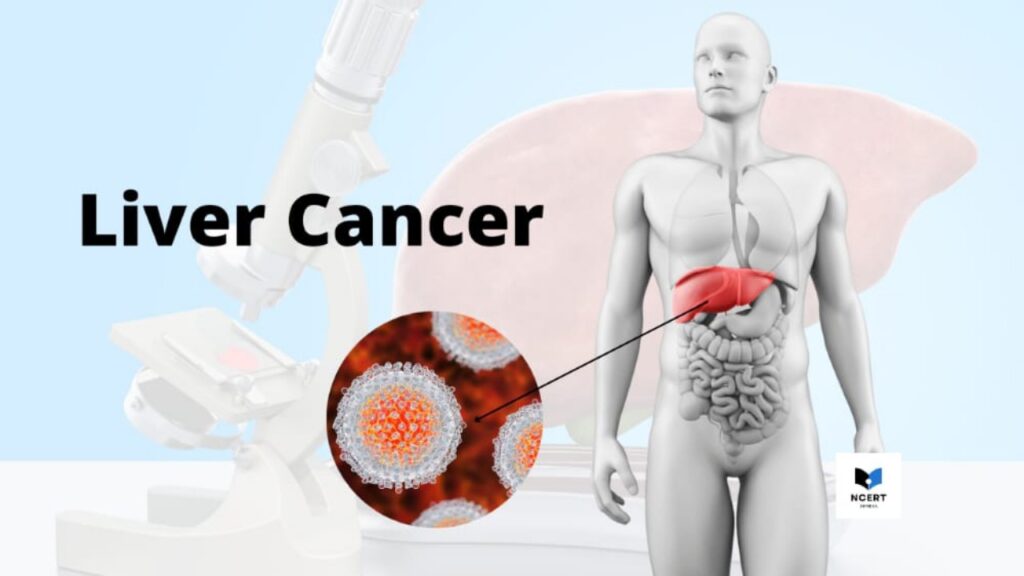
The liver is a football-shaped organ located in the upper right part of your abdomen, below the diaphragm, and above your abdomen. Liver cancer begins in the cells of your liver and destroys them, as well as interfering with liver activity.
There are no specific symptoms in the early stages of liver cancer. As the disease progresses, symptoms related to the liver begin to be felt, such as jaundice.
In most cases, the cause of liver cancer is not known. But in some cases, long-lasting infection of hepatitis causes it.
For its treatment, surgery, chemotherapy, radiation therapy, and targeted drug therapy can be done. Your doctor will decide which of these treatments is right for you.
Liver cancer status in India
It is emerging as the fastest-growing cancer in India. It is estimated to be 3-5 cases per 100,000 people in India, which means 40,000 to 70,000 new cases per year.
However, this figure is expected to be much lower than the actual situation as there is no population-based data due to the absence of a systematic cancer registry in the country.
If we estimate the number of liver cancer patients keeping in mind the number of hepatitis B cases in India, then surely the real picture will be much worse than this.
Liver Cancer Symptoms
Early symptoms
Most people have no symptoms at the beginning of liver cancer. As the condition starts getting worse, the symptoms start to be felt. If you are at high risk of developing liver cancer, keep getting your liver checked regularly.
symptoms and signs
When symptoms of liver cancer begin, they may include the following symptoms:
- Weight loss
- Loss of appetite
- Upper abdominal pain
- Nausea or vomiting
- Weakness and fatigue
- Abdominal bloating
- Feces turning white
Types
There are the following types of liver cancer:
1. Hepatocellular carcinoma (HCC) – Hepatocellular carcinoma, also called hepatoma, is the most common type of liver cancer, accounting for approximately 75 percent of liver cancer cases. HCC begins in the main types of liver cells, which are called hepatocellular cells. Most cases of HCC are due to infection with hepatitis B or C or cirrhosis of the liver caused by alcohol.
2. Fibrolamellar HCC – This is a rare type of HCC that is generally more sensitive to treatment than other types of liver cancer.
3. Bile duct cancer – This cancer occurs in the small, tube-like bile ducts within the liver that connect bile to the gallbladder. It accounts for 10-20% of all liver cancer cases.
4. Angiosarcoma – Angiosarcoma, also known as cholangiocarcinoma, accounts for about 1 percent of liver cancer cases. It starts in the blood vessels and grows quickly.
5. Liver metastasis – This cancer develops when cancer spreads from another part of the body to the liver. Most liver metastases arise from the colon. More than half of people with colorectal cancer also develop liver metastasis.
Stages
There are four stages of liver cancer:
1. First Stage
The first stage of liver cancer means that the tumor has not developed in the blood vessels and the cancer has not spread to nearby lymph nodes or elsewhere.
2. Second Stage
Stage II means the tumor has grown into blood vessels or many small tumors (all smaller than 2 inches) have developed and cancer has not spread to nearby lymph nodes or elsewhere.
3. Third Stage
There are three subtypes of stage III liver cancer:
- First – this means that multiple tumors are present and at least one is larger than 2 inches (5 cm) and the cancer has not spread to nearby lymph nodes or elsewhere.
- Second – this means that multiple tumors are present and that at least one tumor is growing in one branch of the vein and cancer has not spread to nearby lymph nodes or other sites.
- Third – this means that the tumor has spread to a nearby organ (other than the gallbladder) or the outer covering of the liver and has not spread to nearby lymph nodes or other sites.
4. Fourth Stage
Stage IV is the most advanced stage of liver cancer. In this, cancer has spread to nearby lymph nodes and can grow into nearby blood vessels or organs. Advanced liver cancer often does not spread to distant organs, but when it does, it is likely to spread to the lungs and bones.
Causes
It is not usually clear what causes liver cancer. For example, chronic (long-term) infection with certain hepatitis viruses can lead to liver cancer.
It occurs when there are changes in the DNA of liver cells. DNA gives instructions for every chemical process in your body. Changes in DNA cause changes in these instructions. It can also result in cells growing out of control and eventually forming a tumor.
What are the risk factors for liver cancer?
The following are the factors that increase the risk of liver cancer:
- Hepatitis B or C infection – Hepatitis B virus (HBV) or hepatitis C virus (HCV) increase the risk of liver cancer.
- Cirrhosis – Cirrhosis is a progressive and irreversible disease that causes scar tissue to form in your liver and increases your chances of getting liver cancer.
- Certain genetic liver diseases – Certain genetic diseases such as hemochromatosis (excess iron in the body) and Wilson disease increase the risk of liver cancer.
- Non-alcoholic fatty liver – The accumulation of fat in the liver increases the risk of liver cancer.
- Drinking too much alcohol – Consuming alcohol daily for many years can increase the risk of liver damage and liver cancer.
- Obesity – Having a high BMI increases the risk of liver cancer.
Prevention
You can take the following measures to avoid liver cancer:
Avoid cirrhosis – Cirrhosis is a liver lesion and it increases the risk of liver cancer.
- Maintain a healthy weight.
- Use caution when using chemicals.
Get the hepatitis B vaccine – You can reduce your risk of hepatitis B by getting the hepatitis B vaccine, which provides more than 90 percent protection for both adults and children.
Take measures to prevent Hepatitis C – No vaccine exists for Hepatitis C but you can reduce your risk of infection in the following ways –
Do not have sex without knowing the health status of either sexual partner and use a condom every time.
If intravenous medication is needed, make sure the needle is not contaminated before using the needle. Check needles and tools before piercing or tattooing the ear or any other area.
Diagnosis
Diagnosis of liver cancer begins with a medical history examination and physical examination. Be sure to tell your doctor if you have had long-term alcoholism or hepatitis B or C infection.
The diagnostic tests for liver cancer include the following procedures:
Liver function test
Liver function tests help your doctor get a clear picture of the health of your liver by measuring the levels of proteins, liver enzymes, and bilirubin in the blood.
AFP Test
With the AFP test, your doctor determines the health of your liver by measuring the level of proteins in your blood. The presence of alpha-fetoprotein (FP) in the blood can be a sign of liver cancer.
CT or MRI scan
CT scans or MRIs produce detailed images of the liver and other organs in the abdomen (abdomen). These tests can help your doctor determine where the tumor is developing, its size, and whether it has spread to other organs.
Liver biopsy
It is another diagnostic test available for liver cancer. In this, a small piece of liver tissue is removed for examination. You are always sedated to prevent any pain during this procedure.
Liver Cancer Treatment
There is some variation in the treatment for each liver cancer case. This depends on many factors such as the number, size and location of the tumor in the liver, how well the liver is functioning, whether or not the disease has progressed to cirrhosis, and whether the tumor has spread to other organs.
It is treated in the following ways:
Hepatectomy – In hepatectomy, part or all of the liver is removed. Over time, the removed portion increases again.
Liver Transplant – In a liver transplant, the damaged liver of a patient is replaced with a healthy liver. This can only be done if the cancer has not spread to other organs. Medicines are given after the transplant to prevent rejection.
Ablation – Ablation uses heat or ethanol injection to destroy cancer cells. In this, sedation is used so that you do not feel pain. It is beneficial for people who do not have surgery or a transplant.
Chemotherapy – Chemotherapy destroys cancer cells. In this, medicines are given through a vein. Chemotherapy can be effective in treating liver cancer, but many people have other side effects during treatment, including vomiting, loss of appetite, and chills.
Radiation therapy – Radiation therapy uses high-energy radiation rays to kill cancer cells. It has two modes – external radiation and internal radiation.
Targeted drug therapy – Targeted therapy uses specific drugs to kill cancer cells when they are weak. They reduce tumor growth and help to cut off the blood supply to the tumor. It is used for people who have not had a hepatectomy or liver transplant.
Complications
- Jaundice
- Liver failure
- Internal bleeding
- Tremors
- Metastatic liver cancer such as lung cancer and bone cancer